Blocked arteries, also known as arterial blockages or atherosclerosis, occur when plaque — a buildup of fat, cholesterol, and other substances — narrows or obstructs blood flow in the arteries. This can reduce oxygen supply to vital organs and increase the risk of serious cardiovascular events such as heart attacks or strokes. Recognizing the signs of blocked arteries early is essential because many people remain unaware until the condition becomes severe.
While lifestyle factors like poor diet, smoking, and lack of exercise increase risk, genetic predisposition and underlying medical conditions can also contribute. Understanding the warning signs allows for early intervention, potentially preventing serious complications and improving long-term heart health. In this guide, we will explore the key symptoms, risk factors, diagnostic methods, treatment options, and practical steps for prevention.
Table of Contents
- What Are Blocked Arteries?
- Major Causes of Arterial Blockages
- Early Warning Signs of Blocked Arteries
- Symptoms Based on Affected Areas
- How Doctors Diagnose Blocked Arteries
- Treatment and Management Options
- Lifestyle Changes to Reduce Artery Blockage Risk
- 5 Common FAQs About Signs of Blocked Arteries
- Final Thoughts
1. What Are Blocked Arteries?
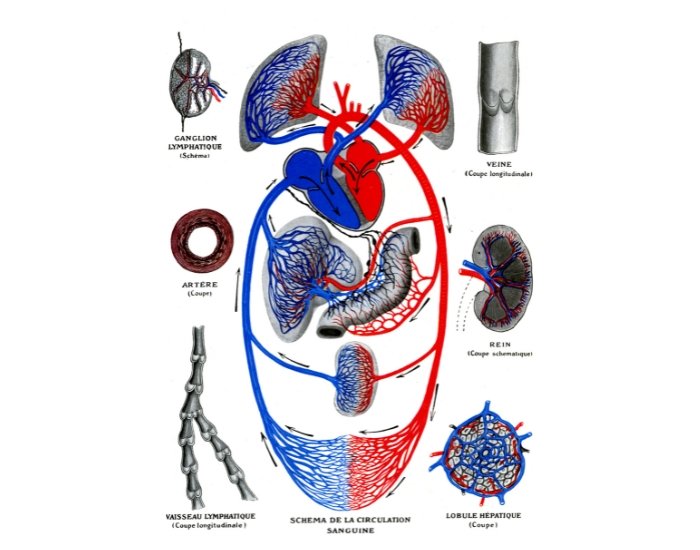
Blocked arteries occur when plaque — a combination of fat, cholesterol, calcium, and other cellular waste — accumulates on artery walls. This buildup narrows the arteries, making it harder for blood to flow through. Over time, restricted blood flow can deprive vital organs of oxygen and nutrients, leading to complications such as heart attacks, strokes, or peripheral artery disease (PAD). Plaque formation is gradual and can start decades before noticeable symptoms appear. Factors like age, family history, smoking, high cholesterol, high blood pressure, diabetes, and obesity all increase the likelihood of arterial blockage. While some blockages are partial and asymptomatic, significant narrowing can trigger warning signs that should never be ignored.
2. Major Causes of Arterial Blockages
Arterial blockages develop over time due to several interconnected causes. The most common include:
- Atherosclerosis: The most prevalent cause, atherosclerosis results from the gradual buildup of plaque in the arteries.
- High Cholesterol: Elevated LDL (bad cholesterol) levels contribute to plaque formation, while low HDL (good cholesterol) reduces the body’s ability to remove excess cholesterol.
- Hypertension: High blood pressure damages arterial walls, making them more susceptible to plaque deposits.
- Smoking: Tobacco smoke accelerates plaque buildup and damages blood vessels.
- Diabetes: Elevated blood sugar levels increase arterial inflammation and plaque accumulation.
- Sedentary Lifestyle and Poor Diet: Lack of physical activity and diets high in saturated fats, sugars, and processed foods contribute to obesity and cardiovascular strain.
Understanding these causes is important because controlling them can significantly reduce the risk of developing severe arterial blockages.
3. Early Warning Signs of Blocked Arteries
Early symptoms of blocked arteries may be subtle or mistaken for fatigue or normal aging. Key warning signs include:
- Chest Pain or Angina: A sensation of pressure, tightness, or burning in the chest, especially during physical activity or stress, can indicate coronary artery blockage.
- Shortness of Breath: Reduced blood flow to the heart may cause difficulty breathing, even during mild exertion.
- Fatigue or Weakness: Oxygen deprivation to muscles and organs may lead to unexplained fatigue.
- Numbness or Weakness in Limbs: Peripheral artery disease can reduce blood flow to legs or arms, causing weakness or tingling sensations.
- Cold Extremities or Poor Wound Healing: Blocked arteries in the limbs can lead to colder hands or feet and slow recovery from injuries.
These signs may appear gradually or suddenly, depending on the location and severity of the blockage.
4. Symptoms Based on Affected Areas
The symptoms of blocked arteries often depend on which part of the body is affected. When the coronary arteries that supply the heart are blocked, people may experience chest discomfort, pressure, or pain, along with shortness of breath, irregular heartbeat, fatigue, and sometimes nausea. If the blockage occurs in the carotid arteries of the neck, which supply the brain, it may lead to sudden weakness, facial drooping, slurred speech, vision changes, or even transient ischemic attacks (mini-strokes). Blockages in the peripheral arteries, particularly in the legs or arms, can cause cramping, numbness, cold extremities, or pain while walking, a condition known as claudication. In cases where the renal arteries to the kidneys are affected, individuals may experience high blood pressure, swelling, fatigue, and in severe situations, impaired kidney function. Recognizing these symptoms in the specific areas of the body can help guide early medical evaluation and prevent complications.
5. How Doctors Diagnose Blocked Arteries
Diagnosing blocked arteries begins with a detailed review of your medical history, risk factors, and current symptoms. Healthcare providers often perform a physical examination and may order blood tests to evaluate cholesterol levels, blood sugar, and other cardiovascular indicators. Imaging techniques, such as CT angiography or MRI, allow doctors to see plaque buildup and the extent of arterial narrowing. For heart-related blockages, an electrocardiogram (ECG) can detect irregular heart rhythms, while an echocardiogram uses ultrasound to visualize heart structure and blood flow. Stress tests may also be conducted to monitor how the heart functions under exertion. By combining these diagnostic tools, doctors can accurately identify the location and severity of blockages and recommend appropriate treatment strategies before serious events like heart attacks or strokes occur.
6. Treatment and Management Options
Treatment depends on the severity and location of the blockage. Mild cases may respond to lifestyle changes and medications, while severe blockages often require medical procedures. Medications may include cholesterol-lowering drugs, blood thinners, beta-blockers, or antihypertensive agents to reduce strain on the heart and improve blood flow. In more severe cases, procedures such as angioplasty, stent placement, or bypass surgery may be recommended to restore proper circulation.
Lifestyle modifications play an equally important role. Adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, managing stress, and controlling underlying conditions like diabetes or high blood pressure can significantly reduce further plaque buildup. Working closely with cardiology experts, such as those at EPIC Heart & Vascular Center, ensures a personalized plan that balances medical intervention with lifestyle strategies.
7. Lifestyle Changes to Reduce Artery Blockage Risk
Even when arterial blockages are detected, lifestyle changes can significantly improve outcomes and prevent further plaque buildup. Adopting a heart-healthy diet that emphasizes fruits, vegetables, whole grains, and lean proteins while limiting saturated fats, processed foods, and sugary drinks is crucial. Regular physical activity, such as walking, cycling, or swimming, helps maintain healthy blood flow, manage weight, and reduce stress on the cardiovascular system. Quitting smoking and limiting alcohol consumption further protect arteries from damage and inflammation. It is also important to monitor key health indicators, including blood pressure, cholesterol, and blood sugar, and to manage stress through techniques like meditation, yoga, or deep breathing exercises. Consistently incorporating these changes can lower the risk of further blockages and improve overall cardiovascular health.
8. 5 Common FAQs About Signs of Blocked Arteries
Q1: What are the early signs of blocked arteries in the heart?
A1: Early signs include chest pressure, shortness of breath, fatigue, and discomfort in the arms or jaw, especially during exertion.
Q2: Can blocked arteries cause leg pain?
A2: Yes. Peripheral artery disease may reduce blood flow to the legs, causing pain, numbness, or cramping during walking.
Q3: How can I know if my arteries are blocked without symptoms?
A3: Blood tests, ECG, stress tests, and imaging studies can detect blockages even before noticeable symptoms appear.
Q4: Are blocked arteries reversible?
A4: While plaque cannot always be completely removed without procedures, medications and lifestyle changes can slow progression and improve blood flow.
Q5: When should I see a doctor for arterial blockage concerns?
A5: If you experience chest pain, shortness of breath, numbness, sudden weakness, or unusual fatigue, seek medical attention immediately.
9. Final Thoughts
Blocked arteries pose a serious risk to cardiovascular health, yet many people remain unaware of the warning signs. Recognizing symptoms, understanding risk factors, and seeking timely evaluation are key steps in preventing life-threatening events. Lifestyle modifications, medical management, and regular monitoring can dramatically improve heart health and reduce future complications. Early detection truly saves lives.
If you or a loved one suspect blocked arteries or want to assess your cardiovascular risk, contact EPIC Heart & Vascular Center today. Our experienced cardiology team provides personalized care, early detection, and effective treatment options to keep your heart and arteries healthy.
Medical Disclaimer: This blog is for educational purposes only and should not replace professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment tailored to your individual needs.